
Here is a list of female sterilization procedures. SterilizationAunty organized them from least invasive to most invasive. The invasiveness depends on a few factors, such as the size of the incision and the amount of material removed. Click the procedure to learn about it in more detail.
By definition, all female sterilization procedures are permanent.
All surgeries can be achieved laparoscopically (minimally invasive surgery) or by laparotomy (open surgery). Very rarely, a female sterilization surgery can be performed through the vaginal opening. There are two discontinued procedures that could be accomplished with a device called a hysteroscope, but we won’t discuss procedures that aren’t performed anymore here.
With all of the listed procedures, having your period on the day of your surgery isn’t a problem. Some doctors have a preference for sterilizing you right after your menstruation because it decreases the chance of you being pregnant during the surgery.
Bilateral tubal ligation (BTL)
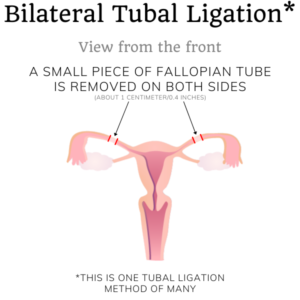
Tubal ligation, also known as tubal occlusion or “having your tubes tied”, is a surgery only prescribed for the purpose of sterilization. The surgeon will make one or more incisions into your abdomen. They’ll find your fallopian tubes and block that passageway. The result is that an egg traveling from your ovary to your uterus won’t be able to reach its destination. From the other end, no sperm cell can travel up your fallopian tube to fertilize the egg.
Bilateral means on both sides; you have two fallopian tubes that both need blocking in order for you to be sterile. Tubal means ‘of the fallopian tubes’; you can find more information about the fallopian tubes on the anatomy page. Ligation means ‘binding’ and occlusion means ‘obstruction’ of the fallopian tubes. Pre-menopausal women of all ages can undergo this surgery.
Bilateral tubal ligation overview table
| Will there be changes in my libido? | No. If there were no complications during the surgery, there will be no changes in your desire for sex. Some women report an improvement in their sex life and satisfaction1 |
| Does it reduce the chance of ovarian cancer? | Yes, by about 34%.2 |
| Will I still menstruate after the procedure? | Yes. You may see decreases in the amount of bleeding, the number of days, and the amount of pain, but an increase in the irregularity.3 |
| Is there a chance of premature menopause? | No, although some people experience menopausal symptoms like hot flashes. |
| What is the failure rate? | About 2% depending on some factors. Younger age correlates with higher failure. Only in the first five years, there’s a risk of failure. If it failed, the pregnancy will almost always be ectopic. |
| Will there be foreign objects in my body? | That depends on the tubal ligation method. There are silicone rubber bands and clips made of a combination of plastic, titanium, stainless steel, gold, and/or silicone.4 |
| Is it reversible? | Assume it’s irreversible. Reversibility depends on the method of tubal ligation. Studies give a large spread of the success rate (38-86%) for reversal.5 Note that these numbers represent pregnancy rates, not birth rates. Don’t get sterilized if you plan on getting pregnant later. |
| Is it compatible with assisted reproductive technology (ART)? | Yes. |
Bilateral salpingectomy (BS)
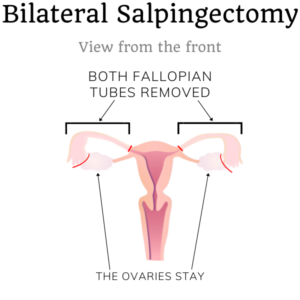
A salpingectomy, also known as a tubectomy, is having your fallopian tubes completely surgically removed. If not the whole tube is removed, it’s called a partial bilateral salpingectomy.
There are many advantages to removing the whole fallopian tube on both sides, but not all surgeons are willing to perform them without a medical reason. This method is slightly more surgically invasive than a bilateral tubal ligation because the surgeon removes more tissue. They will remove everything between the fimbriae and the interstitium.
In this surgery, you’ll keep your ovaries. Preserving your ovaries prevents surgical menopause and loss of libido. If you have a higher risk of ovarian cancer, your doctor might suggest doing a salpingectomy now, and an oophorectomy later in your life. Related words to salpingectomy in the context of ovarian cancer risk are “prophylactic/opportunistic salpingectomy” and “ovarian preservation/ovarian-sparing surgery”. It is often done on younger women who are at risk of developing cancer.
Bilateral salpingectomy overview table
| Will there be changes in my libido? | No. If there were no complications during the surgery, there will be no changes in your desire for sex. Some women report an improvement in their sex life and satisfaction6 |
| Does it reduce the risk of ovarian cancer? | Yes, by up to 50%7 |
| Will I still menstruate after the procedure? | Yes. You may see decreases in the amount of bleeding, the number of days, and the amount of pain, but an increase in the irregularity3 |
| Is there a chance of premature menopause? | No.8 |
| What is the failure rate? | Negligible.9 |
| Will there be foreign objects in my body? | No. The sutures in your body will be dissolvable. |
| Is it reversible? | No. |
| Is it compatible with assisted reproductive technology (ART)? | Yes. |
Bilateral oophorectomy (BO)
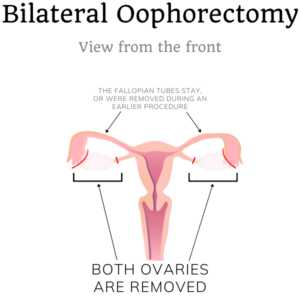
In this procedure, the surgeon will remove your ovaries. An alternative name is “ovariectomy”. Bilateral oophorectomy reduces the risk of ovarian cancer or cysts, and even breast cancer. This is especially true if you test positive for BRCA gene mutations. A doctor can recommend bilateral oophorectomy as a way to prevent such diseases.
A bilateral oophorectomy without a (prior) bilateral salpingectomy is rare; there is no real medical reason to keep the fallopian tubes if you remove the ovaries. Keeping the fallopian tubes may actually not reduce the chance of ovarian cancer as significantly as you’d hope, since ovarian cancer often starts in the fallopian tubes.
Bilateral oophorectomy overview table
| Will there be changes in my libido? | This is very likely.10 |
| Does it reduce the chance of ovarian cancer? | Yes, by about 80–90%11 but not as much as a salpingectomy or combination with a salpingectomy.12 |
| Will I still menstruate after the procedure? | The menstrual cycle will stop. You won’t bleed anymore, especially in combination with a hysterectomy.10 |
| Is there a chance of premature menopause? | Yes, you will enter menopause after the surgery.13((Source: Oophorectomy – Mayo Clinic (2020). You can download the source here.)) |
| What is the failure rate? | No failure. You can’t conceive without at least one ovary.10 |
| Will there be foreign objects in my body? | No. The sutures in your body will be dissolvable. |
| Is it reversible? | No. |
| Is it compatible with assisted reproductive technology (ART)? | It might work.10 |
Bilateral salpingo-oophorectomy (BSO)
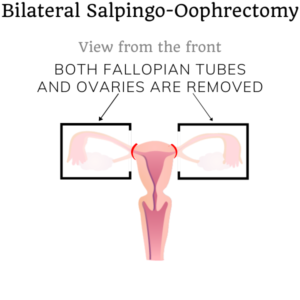
If you’re in a high-risk group for ovarian cancer, your doctor might recommend a bilateral salpingo-oophorectomy. In this surgery, your doctor will remove both the fallopian tubes and the ovaries in one procedure. This surgery is recommended if you’ve tested positive for BRCA gene mutations and are older than 40. If you have such a gene mutation, doing this surgery will also reduce your chances of breast cancer.14
Bilateral salpingo-oophorectomy overview table
| Will there be changes in my libido? | This is very likely.10 |
| Does it reduce the chance of ovarian cancer? | By about 80–96% if you carry the BRCA1 or BRCA2 mutation.14 If you don’t have the mutation, your ovarian cancer risk will virtually be eliminated. |
| Will I still menstruate after the procedure? | No.13 |
| Is there a chance of premature menopause? | Yes, you will enter menopause after the surgery.13((Source: Oophorectomy – Mayo Clinic (2020). You can download the source here.)) |
| What is the failure rate? | No failure. You can’t conceive without at least one ovary.10 |
| Will there be foreign objects in my body? | No. The sutures in your body will be dissolvable. |
| Is it reversible? | No. |
| Is it compatible with assisted reproductive technology (ART)? | It might work.10 |
Hysterectomy (H)
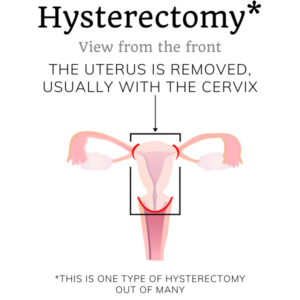
A hysterectomy is the surgical removal of the uterus and sometimes the cervix. Because the uterus is essential to pregnancy, you’ll be sterile afterward. There are many types of hysterectomies and a hysterectomy can be combined with the other procedures listed above.
Surgeons generally won’t perform hysterectomies without a medical reason and trying different options first. If your menstrual bleeding decreases your quality of life, your doctor may prescribe a hysterectomy after first trying pharmacological options and/or endometrial ablation. Another important reason to have a total hysterectomy (uterus and cervix) is to eliminate the risk of cervical cancer.
Hysterectomies are quite invasive.
Hysterectomy overview table
| Will there be changes in my libido? | Depends on whether you keep your ovaries or not. Your sex life might change. |
| Does it reduce the chance of ovarian cancer? | Not without removal of the fallopian tubes and/or ovaries too. |
| Will I still menstruate after the procedure? | No, although spotting may occur from your cervix. |
| Is there a chance of premature menopause? | Depends on if your ovaries are removed as well as your uterus. |
| What is the failure rate? | Negligible.15 |
| Will there be foreign objects in my body? | No. |
| Is it reversible? | No. |
| Is it compatible with assisted reproductive technology (ART)? | No. |
Comparison table of female sterilization surgeries
Here is a quick table with all the previously-mentioned female sterilization surgeries sorted.
| BTL | BS | BO | BSO | H | |
| Is it permanent? | Yes. | Yes. | Yes. | Yes. | Yes. |
| Does libido change? | No. | No. | Yes. | Yes. | No. |
| Ovarian cancer risk reduction? | 34% | 50% | 80–90% | 80–96% | Slightly. |
| Will I menstruate? | Yes. | Yes. | No. | No. | No. |
| Will I enter premature menopause? | No. | No. | Yes. | Yes. | No. |
| What’s the failure rate? | <2% | ~0% | 0% | 0% | ~0% |
| Are there foreign objects in my body? | Maybe. | No. | No. | No. | No. |
| Is it reversible? | Maybe. | No. | No. | No. | No. |
| Is it compatible with ART? | Yes. | Yes. | Maybe. | Maybe. | No. |
- Sources: Raphael, M.B. for the Huffington Post (2014) How my sex life changed when I got my tubes tied. Smith, A. (2010) Are sexual problems more common in women who have had a tubal ligation? A population-based study of Australian women. You can download the study here. Kjer, J.J. (1990) Sexual adjustment to tubal sterilization. Here you can download the study. [↩]
- Source: Cibula, D. et al. (2011) Tubal ligation and the risk of ovarian cancer: review and meta-analysis. You can also download the study here. [↩]
- Source: Peterson, H.B. et al. (2000) The Risk of Menstrual Abnormalities after Tubal Sterilization. You can download the study here [↩] [↩]
- Source: The Clip Project [↩]
- Sources: van Seeters, J.A.H. et al (2017) Tubal anastomosis after previous sterilization: a systematic review. Berger, G.S. et al (2016) Effectiveness of bilateral tubotubal anastomosis in a large outpatient population. La Grange, J. et al (2012) Fallopian tube reanastomosis by laparotomy versus laparoscopy: a meta-analysis. Hanafi, M.M. (2003) Factors affecting the pregnancy rate after microsurgical reversal of tubal ligation. [↩]
- Source: Skorupska, K.A. et al. (2016) Are there any differences in quality of life and sexual functions after various types of hysterectomy – does prophylactic salpingectomy matter? You can download the study here. [↩]
- Source: Balsarkar, G. (2017) Opportunistic Salpingectomy as an Ovarian Cancer Primary Prevention Strategy. You can also download the study. [↩]
- Source: Gillian, E. et al. (2020) Examining indicators of early menopause following opportunistic salpingectomy: a cohort study from British Columbia, Canada. You can download the paper here. [↩]
- Source: Bollapragada, S.S. et al. (2005) Spontaneous pregnancy after bilateral salpingectomy. You can download the case study here.download the case study here [↩]
- Source: Oophorectomy – Mayo Clinic (2020). You can download the source here. [↩] [↩] [↩] [↩] [↩] [↩] [↩]
- Source: Mayo clinic staff (2019) Prophylactic oophorectomy: Preventing cancer by surgically removing your ovaries [↩]
- Source: Parker, W.H. (2014) Oophorectomy or salpingectomy—which makes more sense? You can download the article here. [↩]
- Source: About your bilateral salpingo-oophorectomy – Memorial Sloan Kettering Cancer Center. You can download the procedure guide here [↩] [↩] [↩]
- Source: Kulkarni, A. et al. (2015) Management of Women with a Genetic Predisposition to Gynaecological Cancers. Download the paper here. [↩] [↩]
- Source: Fylstra, D.L. (2015) Ectopic pregnancy after hysterectomy may not be so uncommon: A case report and review of the literature. You can download the case report here. [↩]